In Clinical
Follow this topic
Bookmark
Record learning outcomes
The symptoms associated with diabetes mellitus, a group of metabolic diseases characterised by persistent hyperglycaemia, have been recognised for centuries. Nevertheless, poor knowledge of anatomy and physiology meant the disease remained perplexing to physicians until relatively recently.
As early as 1500 BC, papyrus texts make reference to patients experiencing excessive thirst with copious urination, while ancient Chinese texts mention the sweet urine produced by those with these symptoms.
In the 17th century, English physician Thomas Willis was the first European writer to mention the sweet taste of the urine, and he coined the phrase diabetes mellitus.
However, it was another hundred years before a second physician, Mathew Dobson, actually boiled urine dry and noticed a residual crystalline substance, which he described as tasting like brown sugar.
Fast forward to 1889, and Oskar Minkowski and Joseph von Mering demonstrated that removal of the pancreas in dogs lead to symptoms associated with diabetes.
However, the most significant breakthrough occurred in 1921, with the discovery and purification of insulin. The following year, insulin was successfully used in the treatment of a 14-year-old boy with type 1 diabetes, and in 1923, drug company Eli Lilly became the first manufacturer to mass produce this life-saving hormone for commercial supply.
Pathophysiology
There are two main forms of diabetes mellitus, categorised as either insulin dependent (type 1) or non-insulin dependent (type 2). Globally, type 1 diabetes is estimated to affect 9.5 million people and, in the UK, roughly 90 per cent of children and young people with diabetes have the type 1 form.
The condition commonly first presents in children and young people and becomes lifelong. However, it can occur during adulthood for the first time.
The term ‘diabetes’ comes from the Greek word diabainein, meaning to pass through, in reference to the excessive urination observed in patients. Mellitus is derived from the Latin word mellītus, meaning sweet.
The pancreas is responsible for maintaining blood glucose homeostasis. Housed within the pancreas are a cluster of cells known as the islets of Langerhans comprising two main types of endocrine cells: a central core of beta cells surrounded by alpha cells.
The beta cells release the peptide hormone insulin, which reduces plasma glucose concentrations by stimulating uptake by the liver, skeletal muscle and adipose tissue.
Insulin also suppresses hepatic release of glucose. In contrast, the alpha cells release the hormone glucagon, which raises the concentration of glucose and fatty acids in the bloodstream.
Type 1 diabetes is characterised by destruction of beta cells in an unknown autoimmune process, although the alpha cells are preserved.
This loss of beta cells shows considerable variability. Consequently, some patients have either extremely low or no insulin production at all.
This lack of insulin causes elevation of glucose in the blood (hyperglycaemia) and, in turn, glycosuria (glucose in urine), hence the historical description of sweet urine.
It is now recognised that there are at least three progressive stages in the development of type 1 diabetes, which explains why the condition can develop over a period of months to years.
The underlying cause of the autoimmune process remains unclear, although genetics clearly plays a role since type 1 diabetes is often present in other family members. Despite this, up to 90 per cent of patients do not have another family member with the condition.
Beta cell function can be assessed by measuring levels of connecting peptide (C-peptide), a by-product released by the pancreas when insulin is produced.
Insulin and C-peptide are secreted in a 1:1 ratio in response to oral or intravenous glucose, so measurement of C-peptide provides an assessment of pancreas beta cell function and therefore endogenous insulin production.
Symptoms
The classic signs of type 1 diabetes can appear over a period of days to weeks and include:
- Increased thirst and hunger
- Frequent urination (polyuria)
- Blurred vision
- Increased tiredness and fatigue
- Unexplained weight loss.
Symptoms tend to develop more gradually in adults than they do in children.
Complications
A life-threatening complication is diabetic ketoacidosis (DKA), which is characterised by metabolic acidosis, high levels of ketone bodies (hyperketonaemia) and hyperglycaemia.
DKA can cause a number of symptoms, including nausea, vomiting, polyuria, excessive thirst, fruity smelling breath, tiredness and confusion.
DKA occurs in approximately 30 per cent of people with type 1 diabetes, with up to 55 per cent of children affected and around 6 per cent of adults. It is a medical emergency as it leads to dehydration and electrolyte imbalance.
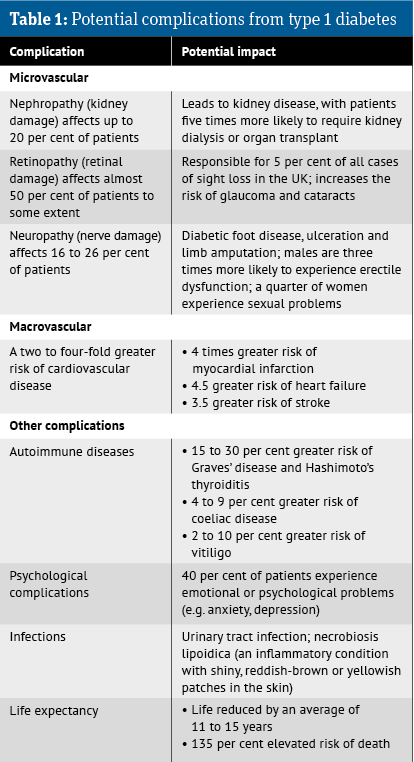
Other complications – see Table 1 below.
Management
Given that the underlying cause of type 1 diabetes is insufficient insulin, the mainstay of treatment involves supplementing with the deficient hormone and patients require life-long insulin replacement therapy.
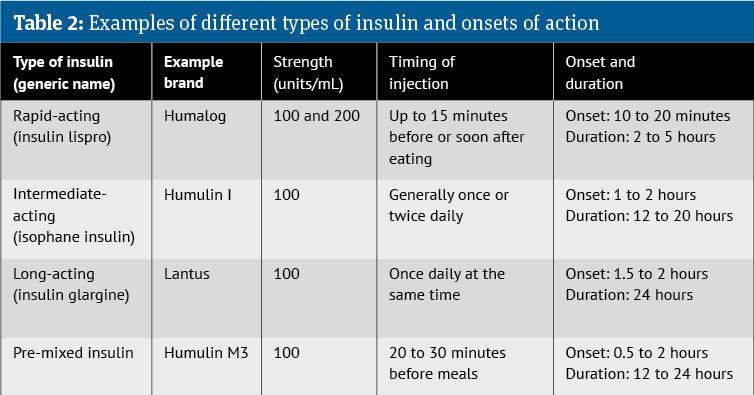
There are a number of different insulin products available. In essence, they can be categorised based on their duration of action into: rapid or short-acting, intermediate-acting, long-acting, and mixed products. A summary of the various types of insulin is provided in Table 2 (below).
More recently, several high strength insulins have become available, with concentrations greater than 100 units/mL for patients with large daily insulin requirements – e.g. Tresiba (200 units/mL) and Toujeo (300 units/mL). This reduces the number of daily injections required.
Insulin administration
Insulin is inactivated by gastrointestinal enzymes, which means it cannot be taken orally. Instead, it is self-administered by subcutaneous injection, generally in areas of the body with plenty of subcutaneous fat, such as the abdomen, outer thighs or buttocks.
Subcutaneous insulin is injected frequently using either a disposable or cartridge refill pen device. When starting on an insulin pen, it is important that patients are shown several devices so that they can find a device that suits them.
Insulin regimens
- Basal-bolus regimen: the primary aim of insulin therapy is to mimic the physiological variation in secretion of insulin. This requires a basal or background level of the hormone, together with spikes that arise following a meal
- Replicating this natural variation in secretion is done with a basal-bolus regimen. This involves using a long-acting insulin to provide a basal level that keeps blood glucose levels stable throughout the day and a bolus, or a single large dose, with a rapid-acting insulin following each meal to prevent a surge in blood glucose
- In its guidance, NICE recommends a basal-bolus regimen first-line for adults and children
- Mixed regimens: by combining a rapid and an intermediate-acting insulin, the regimen is
simplified and can be administered once or twice a day- Such a regimen is suited to those with a regular lifestyle and eating patterns since it has fixed peak action times and durations, allowing patients to inject insulin at relatively consistent times each day
- A disadvantage of the mixed regimen is that the fixed dose insulin combination prevents patients from adjusting the ratio of insulins because of fluctuations in their blood glucose or lifestyle changes
- Insulin pumps: continuous subcutaneous insulin infusion or insulin pump therapy involves a continuous infusion of insulin (usually a rapid-acting insulin), which replaces the basal insulin requirement
- The pump is more flexible and can be programmed to deliver different basal rates of insulin at different times of the day and night. In addition, a higher infusion can be triggered by the push of a button at mealtimes
- Such pumps offer the advantage of matching a patient’s basal requirement, pre-prandial glucose levels, carbohydrate intake and physical activity
- Hybrid closed loop: HCL is the most recent development in continuous infusion technology. It is effectively an artificial pancreas and continuously monitors blood glucose levels via a computer algorithm to automatically adjust insulin delivery
- Manual input is still needed to alert the system when eating or exercising
- NICE has recommended an HCL system as an option for managing blood glucose levels in type 1 diabetes for adults and children who have an HbA1c of 58mmol/mol (7.5 per cent) or more, or disabling hypoglycaemia, despite best possible management.
Resources for type 1 diabetes
- PAM implementation quick guide: england.nhs.uk/wp-content/uploads/2018/04/patient-activation-measure-quick-guide.pdf
- Community Pharmacy England Local Services Database:
cpe.org.uk/lpcs-and-local/locally-commissioned-services/local-services-database - Safe use of insulins: england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Safe-use-of-insulin-and-you-patient-info-booklet.pdf