BPH treatment strategies
Management of BPH typically begins with lifestyle and behavioural modifications for mild symptoms. These include reducing caffeine and alcohol intake, bladder training, pelvic floor exercises, maintaining regular bowel movements, managing weight (target BMI <29) and avoiding symptom-aggravating medications such as antihistamines and decongestants.
Pharmacological treatments include alpha-blockers (e.g. tamsulosin, alfuzosin) for rapid symptom relief, 5-alpha reductase inhibitors (e.g. finasteride, dutasteride) for prostate shrinkage in men with larger glands, and phosphodiesterase-5 inhibitors (e.g. tadalafil) for those with concurrent erectile dysfunction.
Additional options like anticholinergics (e.g. solifenacin) and beta-3 agonists (e.g. mirabegron) target urine storage symptoms by causing the bladder to relax, which helps it to fill, but they should be used cautiously if bladder emptying is poor.
Combination therapies such as alpha-blockers with 5ARIs, anticholinergics or PDE-5 inhibitors are considered for moderate to severe lower urinary tract symptoms or when symptoms overlap.
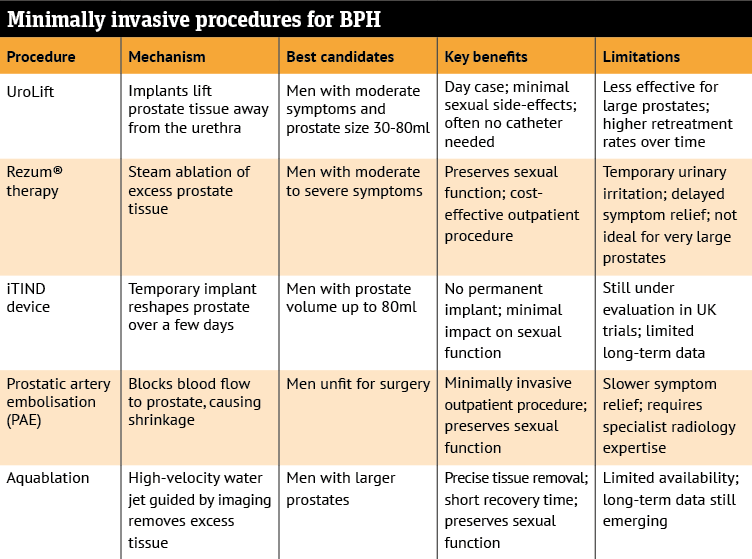
In addition, there are so-called ‘minimally invasive’ procedures for the treatment of BPH. For men experiencing urinary symptoms caused by an enlarged prostate, several treatment options are available that are less invasive than traditional surgery.
These procedures typically offer quicker recovery and aim to preserve sexual function. The table below shows procedure names, mechanisms, best candidates, key benefits and limitations.
These treatments are being compared in UK clinical trials to help determine which option works best for different patient profiles.
The choice of the most suitable treatment is based on individual symptoms, prostate size and overall health of the patient.