Assessing hearing loss
For adults presenting with hearing difficulties where impacted earwax is suspected, there is a need to take a history and examine the ears using an otoscope. If there is no obvious reason for the hearing loss, referral for audiological assessment may be required. Some pharmacies and optometrists offer this assessment, often conducted by a visiting audiologist.
There may sometimes be a need for subsequent urgent onward referral to ear, nose and throat (ENT) services for a small number of patients with certain indications. These include sudden-onset hearing loss, ear discharge in immunocompromised patients, or hearing loss associated with facial ‘droop’ or weakness.
These indications are described further in the NICE guideline (NG98) ‘Hearing loss in adults: assessment and management’.
Examining the patient
Most community pharmacists are acquiring or now have the competencies required for otoscopy. Before examination, the patient should be asked if it is OK to examine them (seeking consent) and hand washing is a prerequisite.
Learning to examine the ear using an otoscope ideally requires supervised training. The more this is practised, the more competent the clinician will be. CPPE has published a list of competencies (see panel opposite).
A normal eardrum (Figure 1) is translucent and greyish in colour. Acute otitis media causes inflammation of the eardrum (Figure 2).
Pharmacists can practise on staff or family members, with their consent, to get familiar with using an otoscope and understand what a range of normal eardrums look like.
There are some useful training resources, such as a short video on how to examine the ear with an otoscope from BMJ Learning. Also available is a link to tympanic membrane (eardrum) diagnostic picture tests.
The otoscope should be held lightly, like a pencil, between thumb, index and middle fingers. The little finger can be rested on the forehead, providing support and allowing movement with the head without knocking the sensitive ear canal. This will need to be repeated with the head held the other way for the other ear.
Increasingly, fibre optic digital otoscopes are used rather than optic lens-based devices. These connect to smart devices via Bluetooth or wi-fi, or are attached directly to the phone, so the eardrum can be visualised on screen.
They have a wide angle of view at the tip and are generally easier to use and less invasive. They must have a UKCE mark and meet MHRA standards.
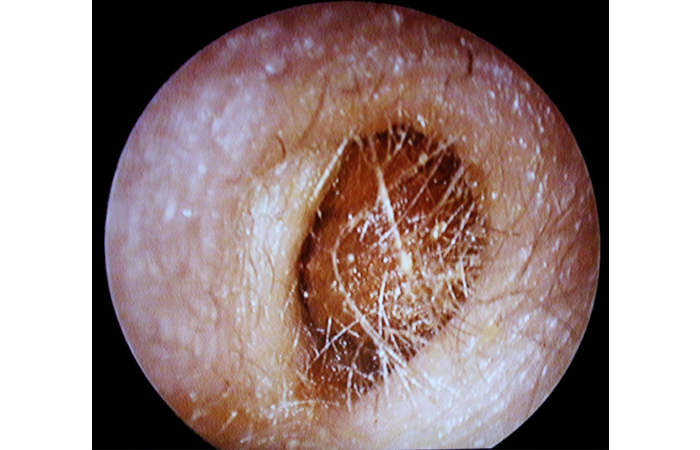
The main impediments to seeing the eardrum clearly are debris or inflammation of the ear canal (usually due to otitis externa), or wax, which appears as a yellowy, orange or brown deposit (see Figure 3).
Identification aid
Left normal ear drum.
Source: ABC of Ear, Nose and Throat edited by Harold Ludman, Patrick J. Bradley. 6th ed, 2013. Wiley. Reproduced with permission of Wiley.
Appearance of eardrum in acute otitis media: inflammation and loss of landmarks. A small amount of yellow earwax is bottom left
Source: Essential Paediatrics and Child Health, 4th ed, 2020. Rudolph M et al. Wiley. Reproduced with permission of Wiley.
Otoscopy of excess earwax
Source: Descouens D. Own work, CC BY-SA 3.0 (commons.wikimedia.org/w/index.php?curid= 8371534)