Acne management
Prompt, effective treatment of acne is important in order to:
- Minimise the risk of long-term scarring
- Reduce the psychological impact.
Effective acne management comprises pharmacological treatment together with supporting advice and guidance. Young people with acne can experience hurtful comments and bullying, and are bombarded with messages about acne that can be confusing. In practice, patients seek treatment when there are obvious inflammatory lesions (i.e. mild-moderate acne).
Community pharmacists and their teams have been advising on acne for many years and are very knowledgeable about OTC treatments.
The 2024 NHS England list of conditions where OTC treatment “should not routinely be prescribed by GPs” includes mild acne as one that should be self-managed with OTC products.
The input of pharmacists is gradually being extended via PGDs and prescribing. These changes will make it possible for community pharmacists to provide a number of effective acne treatments that have hitherto been prescription-only items, so they may need to refresh and update their knowledge of treatments beyond OTCs.
Treatment options
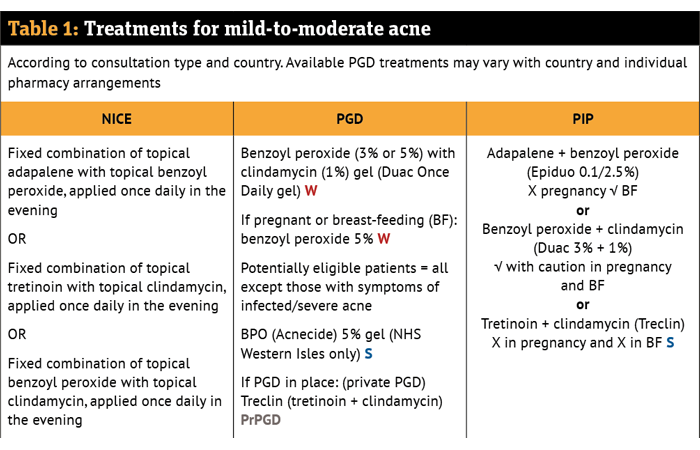
The recommended treatments and current supply options are shown in Table 1. It is appropriate to try OTC treatments for mild and moderate acne where, in the pharmacist’s professional judgement, inflammatory lesions are not widespread, there are no inflammatory nodules and the patient wishes to try an OTC treatment. Benzoyl peroxide (BPO) is the first-line OTC acne treatment.
Where OTC treatment has already been tried for an appropriate length of time or acne severity makes prescription treatment appropriate, NICE guidance recommends first-line treatment with a fixed combination of adapalene + benzoyl peroxide (BPO) or tretinoin + clindamycin or clindamycin + BPO, as these are more effective than the single agents.
They also have the advantage of being easier to apply than two separate products and may be less irritant because lower concentrations of each agent are used than when a product is used alone.
The final choice depends on whether the patient is pregnant (or likely to be) and the degree of irritation experienced with the same ingredients in the past, in addition to patient preference. At present, choice may also depend on availability of appropriate PGDs. Private PGDs are in use as well as NHS PGDs.
In relation to treatment of acne in people with skin of colour, the UK Primary Care Dermatology Society advises: “Topical retinoids, benzoyl peroxide and azelaic acid play an important role in the treatment of the comedonal aspects of acne. If used daily they often cause dryness and irritation, which in skin of colour can lead to further hyperpigmentation.
“Accordingly, these treatments should initially be used for shorter periods of time (e.g. in the evening and washed off before bed) and perhaps less frequently (e.g. every second or third day); if tolerated the duration and/or frequency of treatment can be increased – if used in this way, then as well as treating the comedones they may help treat hyperpigmentation rather than aggravate it.”
See NICE Guideline 198 for full details and rationales for recommended treatments.
W: According to the All Wales Common Ailments Service Formulary, Aug 2023 (updated Jan 2025)
S: According to NHS Pharmacy First Scotland (NHSPFS) (includes Pharmacy First Plus Community Pharmacist IP consultations)
PrPGD: e.g. PGD provided by PharmaDoctor
Private PGDs
For some conditions, off-the-shelf PGDs, together with appropriate training, can be purchased from specialist companies in order to help set up a service. For example, a PGD package for Treclin is available from PharmaDoctor
Key counselling points for acne patients
- Wash the affected area with a mild soap or cleanser and lukewarm water, not more than twice a day. Do not scrub the skin
- Treatments should be applied to the entire affected area of the skin (e.g. all of the face) and not just to individual spots
- Both benzoyl peroxide and retinoids can have drying and irritant effects (redness, peeling, burning, soreness) on the skin. These can be minimised by starting with alternate day or short-contact application (e.g. washing off after an hour)
- Benzoyl peroxide can have a bleaching effect, so avoid getting it on clothes, towels or bedding
- Benzoyl peroxide may cause increased sensitivity to sunlight so avoid exposure and wear sunscreen (oil-free)
- Pus-filled spots (pustules) can be gently squeezed to remove the pus. Other spots must not be squeezed or scratched as this can aggravate them and may cause scarring
- Use oil-free, non-comedogenic cosmetic products (e.g. make-up, suncream), as they are less likely to block the pores in the skin. Remove all make-up before going to bed
- Eat more foods with a lower glycaemic index (fruit and vegetables, brown bread, brown rice, brown pasta)
- Sweat can aggravate acne — shower promptly after exercise
- Sunbathing, sunbeds and sunlamps should not be used to manage acne
- Stopping smoking may help.
Reflection exercise
What four key points would you use when explaining to a patient why it is important to continue using a recommended treatment for the stated length of time?